Medi-Cal Guide for 2021 (California Medicaid)
Medi-Cal is the name for the California Medicaid program. Even though Medicaid itself is a federally-based program, Medicaid allows each state to add its own rules and regulations (to a certain extent). California has adopted its own Medicaid program, Medi-Cal, to serve the specific needs of its residents (32% of which are low-income). In 2019, Medi-Cal California covers two out of every nine California adults, two out of every five California children, and about half of all Californians with disabilities.
This Medi-Cal Guide Includes:
- Med-Cal Eligibility Requirements
- Understanding Medi-Cal Benefits
- Finding Medi-Cal Providers Near You
- Medi-Cal Application
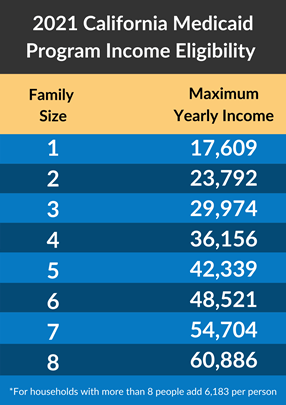
Medi-Cal Eligibility Requirements
The Medi-Cal eligibility requirements are based on your household size and household income. You can generally expect to qualify for Medi-Cal California if your income is at or below 138% of the Federal Poverty Level.
You can also get Medi-Cal if you are:
- 65 or older
- Blind
- Disabled
- Under 21
- Pregnant
- In a skilled nursing or intermediate care home
- On refugee status for a limited time, depending how long you have been in the United States
- A parent or caretaker relative of an age eligible child
- Have been screened for breast and/or cervical cancer (Breast and Cervical Cancer Treatment Program)
If you are enrolled in one of the following programs, you can also get Medi-Cal:
- CalFresh
- SSI/SSP
- CalWorks (AFDC)
- Refugee Assistance
- Foster Care or Adoption Assistance Program
Understanding Medi-Cal Benefits
If you meet the Medi-Cal eligibility requirements, complete the Medi-Cal application! You should hear back within 45 days to know whether or not you’ve gained access to the following Medi-Cal benefits:
- Outpatient and inpatient hospital services
- Emergency room visits and services
- Maternity/Newborn care
- Mental and behavioral health/substance abuse
- Physical and occupational therapy
- Laboratory services
- Preventative & wellness benefits/disease management
- Prescription drugs
- Pediatric medical services (+ dental and vision)
If your Medi-Cal application is approved, you’ll receive information about selecting a plan. Each plan has mostly the same benefits, but individual plans may have some extras. Once you receive it, you have 30 days to select a plan. If you do not select one in time, you will be automatically enrolled in one. Not every plan will be available in every county and zip code. Click here to find the plans available in your county.
*There is only one plan available in San Benito County. You can either enroll in the Anthem Blue Cross Partnership Plan, or you can simply join fee-for-service Medicaid.
The Medi-Cal Dental Benefit
Adults with Medi-Cal California have access to dental exams, x-rays, cleanings, fluoride treatments, fillings, root canals, crowns, dentures, and other medically necessary services. Cosmetic services are not covered. Kids can get all of those service plus orthodontics (if necessary).
Compare Plans from All Carriers in 1 Minute!
California Medicaid Vision & Glasses
Medi-Cal California adults can receive one routine eye exam every two years, but only members under the age of 21 and nursing home residents can receive eyeglass frames and lenses. Contact lenses will only be covered if there is a medical reason that a member needs contacts instead of glasses. Any beneficiary, at any age, may receive artificial eye services if it is medically necessary.
Prescription Coverage and the Medi-Cal Formulary
Need to find out if your prescription will be covered? You can search the Medi-Cal formulary online, here. Just start typing the name of your drug and find out if it’s covered. You can also download a PDF of the Medi-Cal formulary, here.
The good news is that doctors and providers who accept your California Medicaid plan should have the Medi-Cal formulary and only prescribe you drugs that you can get coverage for. Keep in mind that most brand-name drugs have a generic counterpart that works just as well. Medicaid is more likely to cover a generic drug than a brand-name drug, as generics are almost always cheaper.
If a drug you need is not on the Medi-Cal formulary, ask your doctor or pharmacy to submit a TAR (Treatment Authorization Request) to Medi-Cal. Medi-Cal should respond within 24-48 hours to let your pharmacist know if they will cover that medication for you. The same goes for OTC (over-the-counter) drugs. If you need an over-the-counter product but cannot afford it, your doctor or pharmacist can submit a TAR to see if California Medicaid can help you out.

California Medicaid Transportation Benefit
California Medicaid covers both emergency transportation (ambulance) and non-emergency medical transportation. If you do not have a reliable means of transportation and need to get to a California Medicaid-covered appointment, you can contact your plan directly to see if you can schedule someone to come and drive you to your appointment. If your health plan cannot help you directly for any reason, you can email DHCS-Benefits@dhcs.ca.gov. All you need to say is that you need a ride to a medical appointment, and someone will reach back out to ask you for more information. Be sure to schedule your ride at least three days before your appointment, preferably more, to make sure someone can get you there.
Finding Medi-Cal Providers Near You
To take advantage of your Medi-Cal eligibility, be sure to select a doctor who accepts your California Medicaid plan. Using this official Medi-Cal provider search tool is the best way to find a doctor near you who accepts your plan. You can search by provider name if you have a specific doctor in mind. Otherwise, you can search by your health plan, gender, primary language, specialty, and distance from your home.Back to Top
Compare Plans from All Carriers in 1 Minute!
Medi-Cal Application
If you think you meet the Medi-Cal eligibility requirements, it’s time to complete the Medi-Cal application. There are four main ways to apply for Medi-Cal. You can call Covered California at 800-300-1506, you can apply by mail, you can apply in person at a local county human services agency, or you can apply online at CoveredCA.com. Your county should inform you of your eligibility status within about 45 days. If you are approved, you will receive a BIC (benefits identification card) and an informational packet about choosing and enrolling in your Medi-Cal plan.
If you qualify for both Medicaid and Medicare, consider applying for a DSNP. A DSNP, or a dual-eligible special needs plan, is a Medicare Advantage plan specifically for those who are eligible for both Medicare and Medicaid. Having a DSNP might mean even MORE coverage for than Medi-Cal alone.
If you need help sorting through your California Medicare options, complete this form or give us a call 844-431-1832 to get in touch with a licensed agent in California.